Outsourcing in Healthcare Industry
Want to know in detail about the various Healthcare outsourcing services that we provide that can increase profitability? Contact us now, and we'll be delighted to assist you.
MedValue Claims Adjudication and Pended Claims Resolution
Are you being overburdened by pended and unresolved claims?
Claims pended for longer durations increase risk of your organization for health-plan non-compliance, increased support call volume, and lower customer satisfaction.
Experienced Claim Adjudicators
MedValue Claims Adjudication services utilize claims professionals who are trained on multiple adjudication platforms and plan designs. Our Adjudicators have knowledge of medical terminology and are analytical problem solvers. New adjudicators are trained in an intensive program covering the U.S. healthcare industry and claims adjudication. Our claims adjudicators also go through client specific training to learn your insurance plans, systems and claim types.
Our claims processing professionals are trained on multiple claim adjudication systems such as LuminX, Facets, EZ-CAP, and client specific “in-house” custom built adjudication systems, while managing several health plans simultaneously.
Our Diligent Process
Our Claims Examiners review and the process all the claims into these 3 categories:
1. Adjudicated claims
Claims having all the required and relevant information, and result in release of payment to the Provider of healthcare services.
2. Reviewed claims
Denials such as claims that may have exceeded benefit limits, charges incurred after termination date, etc., along with recommended payments and reasons for denial.
3. Correspondence/ Follow up/Provider issue claims
Claims with issues related to pre-existing conditions, accident related subrogation or diagnosis, workers’ compensation claims, license expired physicians, pay-to-provider address mismatch, etc are handled in a separate manner. Our examiners can generate appropriate correspondence from your system to return these claims to the Providers.
MedValue brings you a whole variety of health insurance claims processing solutions to help you manage your claims efficiently. We bring our vast experience of working with healthcare payer claims systems across a variety of technologies.
Key Features
1. Accurately resolve pended claims using your guidelines, state and federal regulations, and using specific health plan criteria.
2. Review attachments and documentation which are received with the claim and utilize that information for adjudication.
3. Correct invalid information and/or enter missing information, so that pended claims are released on a timely basis from your system.
Key Benefits
1. Significant Cost Savings
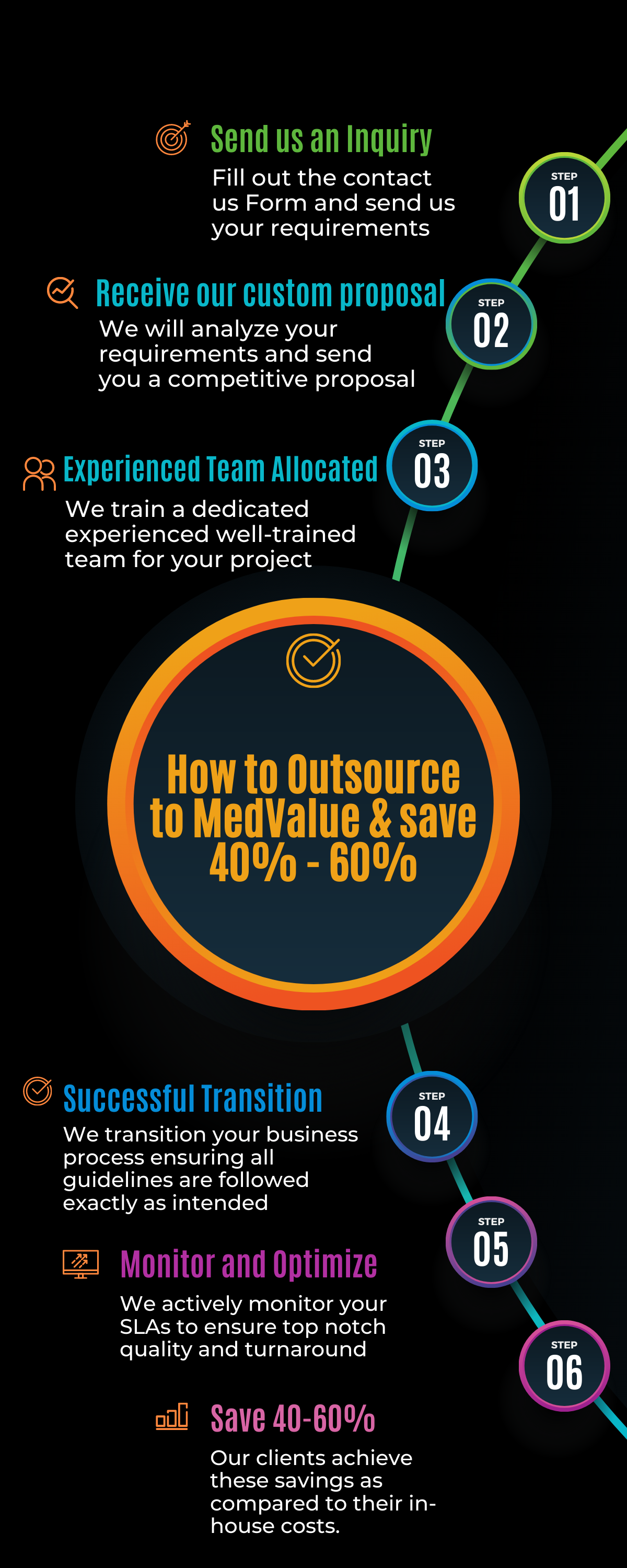
Our Claims Adjudication services provide savings of approximately 40-60% compared to your in-house staff.
2. Better Accuracy
Our claims adjudicators thoroughly review each claim and attachments, resulting in higher accuracy and better compliance with your and health plan guidelines.
3. Improved Customer Satisfaction
Pended claims are resolved on a timely basis resulting in higher customer satisfaction and better plan compliance.
Contact us
Phone Number : 1-877-528-1683